Puberty Blockers for Trans & Non-binary Youth - A Brief Overview
How they work and why they save lives!
Today is trans day of joy, and I wanted to post something that brings joy and euphoria to our trans and non-binary youth who know who they are and want to grow into a body that feels like theirs!
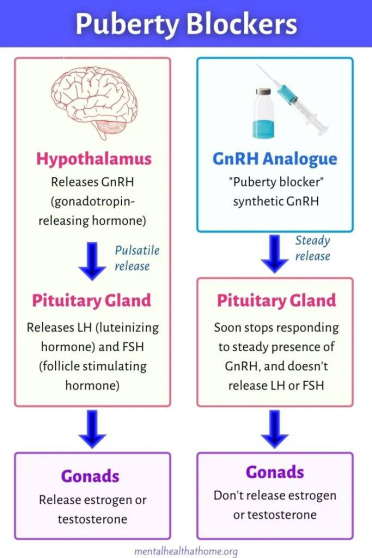
In simple terms, puberty blockers are medications that suppress puberty from happening for a period of time, which stops secondary sexual characteristics from developing. These are things like voice dropping, the start of menstruation, body hair growth and patterns, genital development, Adam’s apples, breast development, or widened hips. Puberty blockers are very safe, and very effective, in youth that are prepubescent or in early stages of puberty.
Puberty blockers have been safely used with cis (or assumed cis) children to treat precocious puberty, the medical term for early puberty, or to treat puberty that is happening too fast for decades! In the US, which is where my experience comes from, puberty blockers are regulated and approved by the FDA, and are extremely well studied in general, mostly on cis children, but more and more studies are looking at trans kids too.
It is very very important to note that folks who have concerns (both valid concerns and antagonistic “concerns”) about the use of puberty blockers are that there are few long-term robust studies conducted for trans youth that take puberty blockers as children and following them through adulthood.
However, long-term studies of cis children from onset to adulthood haven’t been done either, mostly because of the drug safety and doctors seeing the results that children with precocious puberty weren't developmentally altered once they stopped taking the puberty blocker. It only became an issue of major concern when puberty blockers started to be used for trans and non-binary youth, and they are mostly “concerns” pushed by those who are vehemently against any measures that affirm trans lives. Studies on this have exploded with the criticism and scare tactics of trans antagonists demanding a "reason" to deny puberty blockers from gender diverse youth.
There are some conflicting studies as to the dangers of puberty suppression, but most of the differences can be attributed to poor methodology, small sample sizes, or differing ages and duration of treatment with the puberty blocker. The World Professional Association for Transgender Health (WPATH, which is the world authority on trans and non-binary health and takes a neutral stance when looking at a study before critiquing it) notes these studies in their analyses and recommendations. These risks are quite low and are treated easily in most cases (more on this below!).
Puberty blockers are medically called called GnRH analogues. Adults can take GnRH analogues, and are used to treat some forms of breast and prostrate cancer, polycystic ovary syndrome, and endometriosis. Adults taking GnRH analogues have different risk profiles than do for children. These GnRH analogues were prescribed off label since the early 1980's to treat precocious puberty, and the US FDA officially approved them for on-label puberty development since 1993. There are concerns with a specific GnRH analogue called Lupron but studies about that drug do conflict, and the risk profile is higher for adults than for children, and the version of Lupron that children take is specifically for pediatric patients.
The most common puberty blockers (at least in the United States, I cannot speak for other countries) are Goserelin (Zoladex®), Histrelin (Supprelin®LA), Leuprolide (Lupron Depo – Ped®), and Triptorelin (Trelstar®).
Puberty blockers are known to be just as medically safe and effective for both cis kids and for trans and non-binary youth. Potential side effects for all children are a possible loss in bone density, weight gain or loss, acne, irritability, injection site reactions, hot flashes (especially if puberty wasn't suppressed before the onset), and headaches. These symptoms typically go away when puberty is allowed to progress, either through returning to the body’s driving hormone, or a teenager starts HRT.
One risk that is most focused on for children on puberty blockers is bone density. Bone density in all children taking puberty blockers is usually either slightly lower or not statistically different from other children. Typically, youth (cis or non-cis) who have bone density loss are treated with extra vitamin D and calcium, as well as treatments like physical therapy and regular x-rays to monitor bone density changes.
But for most teens and adults who were on puberty blockers as children report that the benefits outweighed the risks, and puberty blockers saved their lives and wellbeing. Being on puberty blockers has shown to be statistically significant that they improve mental health in our youth. Gender dysphoria and suicide rates of trans and non-binary youth plummet when those young people are allowed access to puberty blockers and later, HRT (if they choose that route).
Many trans adults feel like they went through a horrible process with their first puberty, and are stuck with features that would not have developed had they had been given access to puberty blockers early on. This generates huge gender dysphoria, because the body that someone is in does not match their internal sense of self.
If a youth on blockers later determines that they aren’t trans or don’t want to have an alternative puberty, the puberty blocker is stopped and the youth proceeds as typical through puberty for the given driving hormone (estrogen or testosterone).
When a youth reaches teenager status then they and their guardian have a discussion with their doctor to determine if they can start HRT. This is an appropriate time because most youth will have a solid idea of their gender identity at this age, and they can proceed with their correct puberty at an age that is similar to their peers. HRT can have permanent changes, but it is safe to stop. If the teenager isn’t sure, they can remain on puberty blockers up to the age of 18, generally. WPATH updated in their recent revision that HRT can be started as early as 14 or 15, but it's okay to stay on puberty blockers for longer!
If you are considering puberty blockers for your child or if they’ve talked about wanting to start, it is perfectly reasonable and okay to have concerns and gather more information. But I hope this has been helpful for you in understanding the science behind what they do and why they are important!
References:
WPATH Guidelines: https://www.tandfonline.com/doi/pdf/10.1080/26895269.2022.2100644
Turban et. al, 2022, PLOS-One Access, “Access to gender-affirming hormones during adolescence and mental health outcomes among transgender adults https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0261039
Summary of that PLOS One study if this is easier to read: https://fenwayhealth.org/new-study-shows-transgender-people-who-access-gender-affirming-hormones-during-adolescence-are-significantly-less-likely-to-experience-psychological-distress-or-suicidal-ideation/
The Trevor Project about LGBTQIA+ suicide rates https://www.thetrevorproject.org/resources/article/facts-about-lgbtq-youth-suicide/
Article about the WPATH lowering recommendations for HRT to start at age 14 in the most recent edition https://apnews.com/article/gender-transition-treatment-guidelines-9dbe54f670a3a0f5f2831c2bf14f9bbb
Rafferty et. al, 2018, American Academy of Pediatrics “Ensuring Comprehensive Care and Support for Transgender and Gender-Diverse Children and Adolescents” https://publications.aap.org/pediatrics/article/142/4/e20182162/37381/Ensuring-Comprehensive-Care-and-Support-for?autologincheck=redirected
Children's Hospital Boston page: Precocious Early Puberty https://www.childrenshospital.org/conditions/precocious-early-puberty
Cleveland Clinic page: Precocious Puberty/Early Puberty https://my.clevelandclinic.org/health/diseases/21064-precocious-early-puberty
Cleveland Clinic page: “What are Puberty Blockers?” https://health.clevelandclinic.org/what-are-puberty-blockers
GenderGP “Puberty Blockers for Transgender Youth & Bone Health” https://www.gendergp.com/puberty-blockers-bone-health-for-transgender-youth/
Yoo, 2016 Effects of early menarche on physical and psychosocial health problems in adolescent girls and adult women https://www.e-cep.org/journal/view.php?doi=10.3345/kjp.2016.59.9.355
Cohen-Kettenis et. al, 2011, "Puberty Suppression in a Gender-Dysphoric Adolescent: A 22-Year Follow-Up" https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3114100/
McGregor et. al, 2023, Association of Pubertal Blockade at Tanner 2/3 With Psychosocial Benefits in Transgender and Gender Diverse Youth at Hormone Readiness Assessment https://www.sciencedirect.com/science/article/abs/pii/S1054139X23005608